Mastering The 2024 Prior Authorization Process For Medical Providers
0 likes | 16 Views
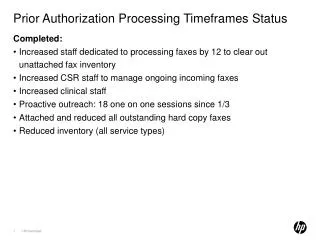
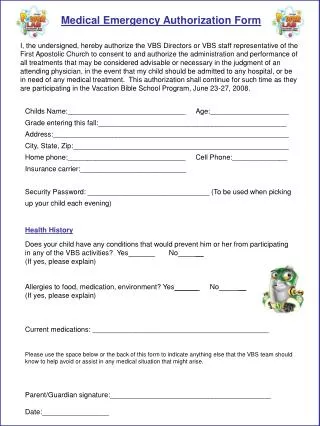
Prior Authorizations are a cost containment strategy that third-party payers leverage to control costs and restrict patient access to services, testing, and medications. In this 60-minute webinar, we will deeply dive into the complexities of the Prior Authorization process, discuss the pearls and pitfalls, define medical necessity requirements, and demystify the intricacies of obtaining prior authorizations, ensuring a smoother workflow and higher approval outcomes in 2024. Register Now, https://conferencepanel.com/conference/mastering-the-2024-prior-authorization-process-for-medical-providers
Download Presentation 

Mastering The 2024 Prior Authorization Process For Medical Providers
An Image/Link below is provided (as is) to download presentation
Download Policy: Content on the Website is provided to you AS IS for your information and personal use and may not be sold / licensed / shared on other websites without getting consent from its author.
Content is provided to you AS IS for your information and personal use only.
Download presentation by click this link.
While downloading, if for some reason you are not able to download a presentation, the publisher may have deleted the file from their server.
During download, if you can't get a presentation, the file might be deleted by the publisher.
E N D
Presentation Transcript
More Related